Table of Contents
At a Glance
|
Migraines are often triggered by things such as certain foods, stress, hormonal shifts, or environmental changes. While all of these can play a role, they do not fully explain what causes migraines or why similar triggers can affect people so differently.
In reality, migraines do not usually have a single cause. Instead, they arise when the brain becomes temporarily overwhelmed through a combination of biological and environmental pressures that push it beyond what it can comfortably manage.
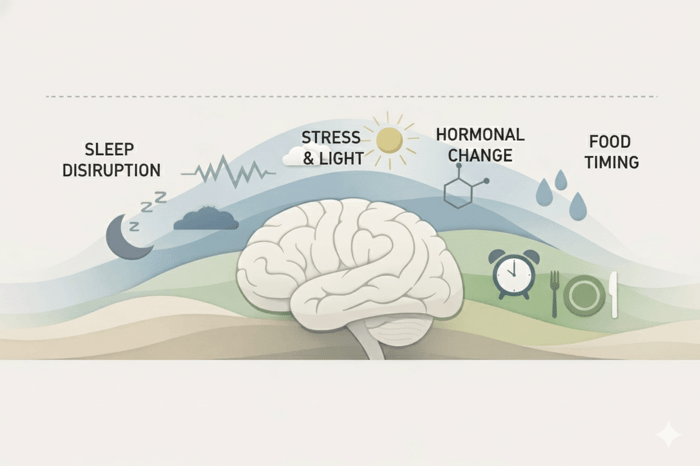
Research increasingly shows that migraine is linked to how the brain regulates energy, processes sensory information, responds to oxidative stress, and adapts to internal change. Factors such as hormonal shifts, disrupted sleep, skipped meals, dehydration, or emotional stress do not cause migraines in isolation. Rather, they place additional demand on systems that already operate under higher baseline strain in people who are migraine-prone.
This helps explain why migraine causes vary so widely between people, and why migraine patterns often shift across different life stages. It also explains why migraines are more likely to emerge during periods of rapid change rather than during stable conditions.
This article explores what causes migraines at a systems level, then examines how those causes can differ across migraine subtypes, biological sex, age, and life stages.
What Causes Migraines? The Core Mechanisms
Migraine research increasingly points to a shared set of underlying mechanisms that influence how the brain manages energy, processes sensory input, and responds to physiological stress (Ferrari et al., 2022). When instability develops across these interconnected systems, migraine activity is more likely to emerge.

One of the most important factors is brain energy metabolism. The brain requires a constant and reliable supply of energy to maintain electrical signaling, regulate neurotransmitters, and support normal sensory processing. In people who are migraine-prone, these energy systems appear to operate closer to their limits. When demand rises, such as during stress, poor sleep, illness, or missed meals, the brain may struggle to meet its energy needs, increasing vulnerability to migraine.
Closely linked to energy metabolism is sensory processing sensitivity. Brains that are prone to migraine tend to respond more strongly to light, sound, movement, and other sensory signals. This heightened responsiveness reflects differences in how sensory thresholds are regulated, particularly in the visual and sensory cortex. When these thresholds are exceeded, even everyday stimuli can contribute to overload rather than being efficiently filtered out.
Oxidative stress is another key mechanism in migraine. Normal brain activity produces reactive byproducts that must be neutralized by antioxidant systems to maintain cellular stability. When antioxidant capacity is reduced, or when oxidative load increases, cellular stress can rise and place additional strain on energy-producing pathways. In brains susceptible to migraines, this imbalance may impair mitochondrial function and neural stability, lowering the threshold at which migraine activity is triggered (Amiri et al., 2022).
Migraine is also associated with changes in neurovascular signaling, the communication between nerve cells and blood vessels. These changes reflect altered regulation of blood flow in response to neural activity. Disruptions in this signaling can influence pain pathways, sensory sensitivity, and aura-related symptoms.
In addition to neurovascular changes, migraine is linked to inflammatory and neurochemical signaling within the brain. Fluctuations in neurotransmitters such as serotonin, along with immune-related signaling molecules, can influence pain pathways, vascular responses, and sensory sensitivity. These processes often interact with energy metabolism and oxidative stress, contributing to cumulative neurological strain rather than acting alone.
Migraines are more likely to occur during times of rapid change than when conditions are stable. Sudden hormonal shifts, abrupt sleep disruption, quick changes in routine, or sharp increases in stress can all place disproportionate strain on interconnected systems. In contrast, steady states, even if imperfect, are often better tolerated by the migraine-prone brain.
Taken together, these mechanisms help explain why migraines arise through cumulative pressure across multiple systems, with isolated triggers playing a more limited role (Grech et al., 2021).
Common Triggers That Can Cause Migraines
Although migraines are shaped by underlying biological vulnerabilities, certain external and internal factors help explain what causes migraines to emerge more readily in everyday life. These triggers rarely act on their own and tend to place additional strain on systems that are already operating close to their limits.
Energy and metabolic stressors
Disrupted sleep, missed meals, dehydration, and irregular eating patterns are among the most commonly reported migraine triggers. These disruptions can interfere with the brain’s ability to maintain a stable energy supply and metabolic balance. Inconsistent energy availability can disrupt neural signaling and sensory processing, increasing susceptibility to migraine during busy or physically demanding periods.
Sensory and environmental load
Bright light, prolonged screen use, loud environments, strong smells, and changes in weather or barometric pressure can all contribute to sensory overload. In brains susceptible to migraine, sensory filtering mechanisms are often less effective, allowing everyday stimuli to accumulate rather than being processed smoothly. Over time, this increased sensory load can contribute to migraine onset, particularly when combined with other stressors.
Psychological and physiological stress
Emotional stress, illness, and physical strain can place additional demand on the body’s stress-response systems. Migraines can occur during sustained stress and during phases of stress release, when the nervous system is adjusting back toward baseline. These shifts can temporarily destabilize energy regulation, vascular signaling, and sensory thresholds, increasing the likelihood of migraine.
Dietary compounds and medication effects
Certain food components, additives, and medications may act as triggers by influencing neurotransmitter activity, blood vessel signaling, metabolic pathways, and processes involved in energy regulation and cellular stress. Caffeine withdrawal, medication overuse, and sensitivity to specific dietary compounds can all contribute to cumulative strain rather than acting as direct causes on their own.
For a more detailed breakdown of specific triggers and how they interact, see our full guide to migraine triggers.
Migraine Subtypes and Variants
Migraine can present itself in several distinct forms. These differences reflect how underlying neurological mechanisms are expressed. While these subtypes may look different on the surface, they are rooted in the same underlying brain processes. The following sections look at how those shared mechanisms relate to different migraine variants.
What Causes Ocular Migraines?
Ocular migraines are primarily associated with transient visual disturbances affecting one eye. Mechanistically, they involve altered signaling within visual processing pathways that regulate blood flow and neural activity in response to visual input. Changes in neurovascular signaling along with heightened sensory sensitivity may temporarily disrupt normal visual processing. These disruptions are more likely to occur when energy availability is strained or during periods of rapid physiological change.
What Causes Optical Migraine or Aura Migraines?
Migraine with aura, sometimes referred to as optical migraine when visual symptoms are prominent, is associated with temporary changes in cortical excitability, particularly within visual and sensory regions of the brain. Mechanistically, these episodes involve waves of altered neural activity that affect how sensory information is processed. Shifts in energy metabolism, oxidative stress, and neurovascular signaling can lower the threshold for abnormal sensory signaling. Aura symptoms are more likely to emerge when multiple systems are under simultaneous strain, which helps explain why visual disturbances can occur before or alongside migraine pain.
What Causes Silent Migraines?
Silent migraines occur when migraine-related neurological activity develops without significant head pain. Symptoms can include visual, sensory, or cognitive disturbances similar to migraine with aura, but without the characteristic headache. Mechanistically, changes in sensory processing, cortical signaling, or neurovascular regulation can still take place, while pain pathways are less strongly engaged. This reflects the fact that migraine is not defined solely by headache, but by broader changes in brain function. Silent migraines are more likely to emerge when these underlying systems are affected without fully activating pain responses.
Life Stage and Biological Differences
Migraine patterns can vary across life stages and between individuals due to differences in biology, hormone regulation, and nervous system development. While underlying mechanisms remain consistent, when and how migraine activity emerges is often shaped by physiological context.
What Causes Migraines in Men?
In men, migraines are often linked to disruptions in energy regulation, sleep patterns, stress responses, and sensory processing rather than hormonal fluctuations. Migraines are often under-recognized in men because symptoms do not always fit stereotypical patterns that emphasize hormonal triggers. Migraine susceptibility may increase when physical strain, irregular routines, dehydration, and prolonged sensory load place added pressure on neurological systems. Changes in stress-response signaling and vascular regulation may also play a role in men, particularly during periods of sustained workload or recovery from stress.
What Causes Migraines in Females?
In women, migraines are strongly influenced by hormonal dynamics, particularly fluctuations in estrogen, which interact with shared underlying neurological systems. Rapid hormonal shifts can affect energy metabolism, antioxidant capacity, and sensory thresholds, making migraine activity more likely during certain phases of the menstrual cycle. These effects may be amplified during life stages such as puberty, perimenopause, or menopause, when hormonal regulation is less stable. While hormones do not directly cause migraines, rapid hormonal fluctuations can lower the threshold at which underlying neurological mechanisms become overwhelmed.
What Causes Migraines During Pregnancy?
During pregnancy, migraines may change in frequency or severity due to substantial physiological adaptation. Increased energy demands, changes in circulating blood volume, disrupted sleep patterns, and changes in hormone levels can all influence migraine susceptibility. Some people experience improvement in migraine symptoms as hormonal patterns stabilize, while others may notice new or worsening symptoms during times of rapid physiological change in pregnancy. Migraine activity during this period reflects how the brain adapts to sustained metabolic and neurological demands rather than a single causal factor.
What Causes Migraines in Children?
In children, migraine is closely linked to nervous system development and energy regulation. Migraine activity often presents differently than in adults, sometimes occurring without head pain. Variants such as abdominal migraine reflect how migraine-related neurological signaling can be expressed through other systems during development. Irregular sleep, missed meals, sensory overload, and stress can all contribute to migraine susceptibility as regulatory systems mature.
Why Migraine Causes Differ Between People
Migraine causes differ between people because migraine activity reflects individual neurological thresholds rather than responses to specific triggers. This threshold reflects how well the brain regulates energy, processes sensory input, manages stress, and adapts to change.
Some people have a baseline that sits closer to this threshold, meaning smaller disruptions can be enough to trigger migraine activity, while others have greater buffering capacity and require more cumulative strain before symptoms emerge. Genetics, sleep and eating patterns, hormonal rhythms, and daily factors such as food choices and sensory input all influence where an individual threshold sits.
Your genetics contribute to this picture by shaping how these systems function and how resilient they are. Rather than determining a single cause, genetic differences influence how easily migraine activity can be triggered in everyday life.
Supporting Migraine Resilience with Brain Ritual®
Because migraine activity is closely tied to energy regulation, oxidative stress, and overall neurological resilience, nutritional strategies that support these systems may help reduce cumulative strain over time. For some, a more focused nutritional approach can offer additional support.
Brain Ritual® was developed as a medical food to support the dietary management of migraine by addressing several of the core mechanisms discussed above. Its formulation includes D-beta-hydroxybutyrate (BHB), a ketone body that provides an efficient alternative fuel source for the brain, helping support energy availability when metabolic demand is high. Ketones may be particularly relevant during periods of stress, disrupted eating, or hormonal change, when glucose-based energy pathways can become less reliable.
The formula also includes nutrients involved in mitochondrial function and antioxidant support, such as magnesium, riboflavin (vitamin B2), and CoQ10, alongside L-carnitine to support energy metabolism and taurine for cellular and neurological stability. Together, these nutrients help support the brain’s ability to manage oxidative load and maintain more stable energy production under demand.
Rather than targeting specific triggers, Brain Ritual® is designed to support the systems that influence where an individual migraine threshold sits, with the aim of improving resilience across everyday conditions.
To learn more about Brain Ritual® and its full formulation, visit our product page here: https://www.brainritual.com/pages/purchase
Disclaimer: Brain Ritual® is a medical food for the dietary management of migraine and is not intended to diagnose, treat, cure, or prevent any disease. This content is for informational and educational purposes only and is not intended as medical advice.
Final Thoughts
Understanding what causes migraines becomes easier when you move beyond individual triggers and look at how the brain functions as a whole. Migraine activity reflects how well core systems involved in energy regulation, sensory processing, stress response, and adaptation are supported over time. When these systems are under sustained pressure, migraine activity becomes more likely.
Viewing migraine in this way can reduce confusion, shifting the focus away from avoiding individual triggers and toward supporting overall neurological resilience. It also helps explain why the causes of migraines vary between people and across life stages. Taking time to explore migraine types, life-stage influences, and trigger patterns can help build a clearer and more manageable understanding of migraine.