At a Glance
|
That familiar throbbing pain strikes again, leaving you wondering: "Are migraines hereditary, or is it just bad luck?"
If you've watched your mother retreat to a dark room with an ice pack, only to find yourself doing the same years later, you're not imagining the connection.
The truth? Your family tree may be partly responsible for those debilitating headaches.
About 34-64% of migraine sufferers can point to a relative who shares their pain, but here's the empowering part: inheriting migraine genes doesn't sentence you to a lifetime of suffering.

In this article, we'll decode the fascinating science behind why migraines run in families, reveal the surprising maternal connection many don't know about, and, most importantly, show you proven strategies to break the cycle, even with migraine-prone DNA.
Your genes might load the gun, but YOU control whether it fires.
How Genetics Shape the Migraine Puzzle
Let's unravel how your genetic blueprint influences your migraine destiny, and why this knowledge is crucial for breaking free from the cycle.
Decoding your migraine genetic blueprint
If your mother, father, or siblings deal with migraine, your chances of experiencing them increase significantly.
This family pattern has been observed consistently across multiple studies, making family history one of the strongest predictors of whether you'll develop a migraine yourself.
What makes this family connection so important is that it often extends beyond just getting a migraine, the specific symptoms, triggers, and even response to protocols can sometimes mirror what your relatives experience.
For example, if your mother's migraine was triggered by certain foods or came with visual auras, you might notice similar patterns in your own attacks.
Your genetic blueprint for migraine comes from two distinct sources within your cells that work in different ways:
Genetic Source | Inheritance Pattern | Key Migraine Impacts | Notable Genes/Factors |
Nuclear DNA | Inherited equally from both parents | Affects brain cell communication, neuron firing, and sensitivity to triggers | CACNA1A, ATP1A2, SCN1A (especially in familial hemiplegic migraine) |
Mitochondrial DNA | Inherited exclusively from mother | Influences cellular energy production efficiency in brain cells | Affects brain's energy metabolism and threshold for triggering attacks |
These genetic variations often affect how your brain cells communicate.
Some impact calcium channels that control how neurons fire, while others influence neurotransmitter systems or ion transport across cell membranes.
The result? A brain that's more sensitive to normal environmental changes and more likely to initiate the cascade of events that lead to a migraine attack.
Particularly fascinating is how researchers have identified specific genes like CACNA1A, ATP1A2, and SCN1A that, when mutated, dramatically increase migraine risk.
These genes essentially make your brain's electrical system more easily "triggered" by ordinary stimuli that wouldn't bother someone without these genetic variations.
Why migraine often passes down the mother's line
Have you noticed migraines seem to pass more frequently from mothers to their children?
There's a biological reason for this pattern, and it revolves around mitochondria, those tiny powerhouses inside your cells that generate energy for all cellular processes.
Unlike nuclear DNA, mitochondrial DNA comes exclusively from your mother.
This maternal inheritance pattern helps explain why migraine sometimes appears to travel down the maternal line more strongly.
When a mother passes on mitochondrial DNA with subtle defects, it affects how efficiently her children's cells, particularly their brain cells, produce and use energy.
This maternal connection becomes especially important because brain tissue is extremely energy-hungry.
When your mitochondria don't work optimally, your brain becomes more vulnerable to energy deficits, which can directly trigger migraine attacks.
This is why some families see generation after generation of women experiencing similar migraine patterns, though of course men inherit this mitochondrial DNA too and can certainly suffer from migraine as well.
How Mitochondria and Triggers Set Off the Storm
Understanding migraine means looking beyond genetics to the cellular level, where the real action happens.

Your body's energy factories, mitochondria, play a starring role in this neurological drama, while everyday factors from your environment act as the supporting cast.
This dynamic interaction explains why you might get migraine on some days but not others, and more importantly, reveals opportunities to intervene before pain strikes.
How faulty mitochondria can amplify migraine risk
Imagine your brain cells as high-performance vehicles that need premium fuel to run properly.
Mitochondria are the engines that convert nutrients into that fuel (ATP), and when these engines don't work efficiently, everything suffers, especially your brain's ability to handle stress.
In migraine-prone individuals, mitochondria often don't produce energy optimally.
This creates a lower threshold for what your brain can handle before triggering a migraine.
When your cells' energy-producing structures (mitochondria) aren't working properly, they generate more harmful waste products like free radicals, leading to oxidative stress.
Oxidative stress can trigger processes that promote inflammation and alter blood vessels, which are important features of migraine attacks.
What makes this situation particularly challenging is that the brain consumes about 20% of your body's energy despite being only 2% of your body weight.
With faulty mitochondria, even normal activities can sometimes push your brain into an energy deficit, essentially forcing it to operate in "emergency mode", and that emergency response often includes a migraine.
Common lifestyle and environmental triggers
While your genes set the stage for migraine, everyday factors pull the trigger.
Think of your migraine threshold as a cup that gradually fills with water.
Genetic predisposition determines the size of your cup, while triggers are the drops that eventually make it overflow.
Some of the most common triggers include:
Sleep disruptions: Both too little and too much sleep can trigger migraine, making consistent sleep schedules crucial.
Dietary factors: Certain foods and additives like aged cheeses, processed meats, MSG, artificial sweeteners, sugar, processed foods and alcohol (especially red wine) are notorious triggers.
Skipped meals: When you fast or delay eating, blood sugar fluctuations can rapidly deplete your brain's energy reserves.
Weather changes: Barometric pressure shifts, sudden temperature changes, and storms can trigger migraine in sensitive individuals.
Sensory overload: Bright or flickering lights, strong smells, and loud noises can overwhelm an already sensitive brain.
Physical exertion: Intense exercise without proper preparation or hydration can create an energy deficit.
What makes triggers particularly tricky is that they're cumulative.
On a good day, you might handle bright lights without problems, but combine that with stress and skipping lunch, and you've exceeded your threshold.
How hormones and metabolism play a hidden role
For many migraine sufferers, particularly women, hormones act as powerful behind-the-scenes influencers.
Estrogen fluctuations dramatically affect migraine frequency and severity.
Many women experience their worst migraine just before or during menstruation when estrogen levels drop rapidly.
This explains why migraine often begins around puberty, changes during pregnancy (improving for many women), and sometimes resolves after menopause.
Estrogen’s influence extends to the mitochondria as well, as it helps regulate mitochondrial function and energy production within cells.
When estrogen levels fluctuate significantly, mitochondrial efficiency can decrease and oxidative stress may increase, contributing to the conditions that can trigger migraine attacks
Beyond sex hormones, your overall metabolism affects migraine vulnerability.
Insulin resistance, blood sugar instability, and other metabolic issues directly impact how well your brain cells function.
This is why conditions like diabetes and metabolic syndrome often coexist with migraine disorders, they all reflect underlying issues with how your body processes and uses energy.
How You Can Break the Cycle and Take Control
The most empowering truth about hereditary migraine is that genes aren't destiny.
While your DNA may load the gun, your lifestyle choices determine whether it fires.
Armed with modern research and a growing arsenal of protocols, you can rewrite your migraine story, even if everyone in your family has suffered for generations.
These evidence-based strategies offer real hope for fewer attacks and milder symptoms, putting you back in charge of your health.
Boosting mitochondrial health with smart choices
Given the crucial role mitochondria play in migraine susceptibility, supporting these cellular powerhouses can be a game-changer in breaking the hereditary cycle.
Medical food Brain Ritual stands apart as the world's first migraine-specific metabolic support formula.

Developed by neuroscientist Dr. Elena Gross, it addresses what researchers believe to be a root cause for migraine sufferers: suboptimal brain metabolism.
The formula's key innovation is providing ketone bodies (primarily D-Beta-Hydroxybutyrate) that serve as an alternative energy source for brain cells.
This bypasses the glucose-dependent metabolism often impaired in migraine sufferers.
By combining these ketone bodies with CoQ10, L-Carnitine, and other mitochondrial-supporting nutrients, Brain Ritual creates a comprehensive approach to improving cellular energy production.
Below we will compare some of mitochondrial support options:
Approach | Key Components | Benefits | Evidence Strength |
Brain Ritual | Ketone bodies (D-BHB), CoQ10, L-Carnitine along with comprehensive formula. See this page for a full list of ingredients and how it works. | • Alternative brain fuel source | Clinical support for targeting migraine-specific metabolic issues |
CoQ10 | Coenzyme Q10 | • Helps generate cellular energy | Multiple positive clinical trials |
Riboflavin (B2) | Vitamin B2 | • Precursor for energy production | Decent research support |
Magnesium | Magnesium glycinate or threonate | • Supports 300+ biochemical reactions | Strong evidence (50% of migraine sufferers deficient) |
Dietary Approaches | Antioxidant-rich foods, Omega-3 fatty acids | • Combats oxidative stress | Supportive research as complementary strategy |
The good news is that even if you inherited less-than-ideal mitochondrial DNA, these research-backed strategies can help optimize your cellular energy production.
While individual supplements show promise, Brain Ritual's comprehensive approach specifically targets the unique metabolic deficits seen in migraine sufferers and it may potentially offer superior results for those with hereditary migraine patterns.
Lifestyle shifts that manage migraine triggers
Breaking the cycle of inherited migraine often comes down to consistent lifestyle practices that keep you below your trigger threshold.
Think of this as maintenance for your brain.
Sleep quality and consistency rank among the most powerful interventions. Going to bed and waking at the same time daily, even on weekends, helps regulate your brain's internal clock and energy usage patterns.
Creating a dark, cool sleep environment and avoiding screens before bedtime produces more restorative sleep that allows your brain to properly recover.
Hydration status dramatically affects migraine susceptibility, as even mild dehydration can trigger attacks in predisposed individuals.
Rather than waiting until you feel thirsty, aim to drink water consistently throughout the day.
A good target for many people is about 2-3 liters daily, more if you're exercising or in hot weather.
Regular, moderate exercise provides a two-fold benefit: it improves mitochondrial efficiency over time while also reducing stress.
The key is consistency without overdoing it. Start with gentle options like walking, swimming, or yoga and gradually build intensity.
For some migraine sufferers, very intense exercise can initially trigger attacks, so finding your personal balance is crucial.
Stress management deserves special attention, as chronic stress creates a perfect storm for migraine activation.
Techniques like mindfulness meditation, deep breathing, and progressive muscle relaxation directly counter the physiological stress response.
Even brief daily practices of 10-15 minutes can lower migraine frequency when done consistently.
Meal timing and composition strongly influence brain energy levels.
Rather than three large meals, many migraine sufferers benefit from eating smaller, balanced meals every 3-4 hours to minimize blood sugar fluctuations.
Including protein and healthy fats with each meal slows digestion and provides more stable energy to your brain.
Medical approaches that can lower attacks
While lifestyle modifications form the foundation of breaking the hereditary migraine cycle, medical interventions can provide crucial support, especially for those with frequent or severe attacks.
Medications, taken regularly to lower attack frequency, have evolved significantly in recent years.
Traditional options include beta-blockers, anticonvulsants, and certain antidepressants, all of which work by stabilizing neuronal activity.
The newest additions to this arsenal are CGRP antagonists, medications specifically designed to block the calcitonin gene-related peptide, a key player in migraine pain.
These monthly injections or quarterly infusions have shown remarkable results even in people who did not respond to other approaches.
For hormonally-triggered migraine, working with healthcare providers to address the underlying pattern can be transformative.
Options range from continuous birth control pills (which eliminate the estrogen drops that trigger menstrual migraine) to hormone replacement therapy during perimenopause.
The key is finding the right hormonal balance for your individual biochemistry.
Neuromodulation devices represent an exciting frontier in migraine management.
These non-drug approaches use electrical or magnetic stimulation to alter brain activity.
FDA-approved options include devices that stimulate the trigeminal nerve, vagus nerve, or create magnetic pulses that can both minimize migraine and abort attacks in progress.
Botulinum toxin (Botox) injections have been proven for chronic migraine sufferers, minimizing headache days by 50% in many patients.
Administered every three months, these injections work by blocking pain signals in nerve endings around the head and neck.
Perhaps most importantly, working with healthcare providers who understand the genetic and mitochondrial components of migraine can lead to more personalized plans.
Genetic testing, while still evolving in this field, may eventually help predict which protocols will work best for your specific migraine pattern.
The bottom line is clear: while you can't change your genetic inheritance, you absolutely can influence how those genes express themselves.
Through targeted mitochondrial support, consistent lifestyle practices that respect your personal thresholds, and appropriate medical interventions, many individuals with hereditary migraine can experience a substantial reduction in the frequency and severity of attacks—sometimes up to 50% or more—though individual results vary.
This means that even with a strong family history of migraine, you aren't destined to follow the same painful path as your relatives.
You have more power to rewrite your migraine story than you might have thought possible.
Frequently Asked Questions
After exploring the above insights, you might still have some lingering questions, so we will address a few of the most common queries regarding migraine and their hereditary nature.
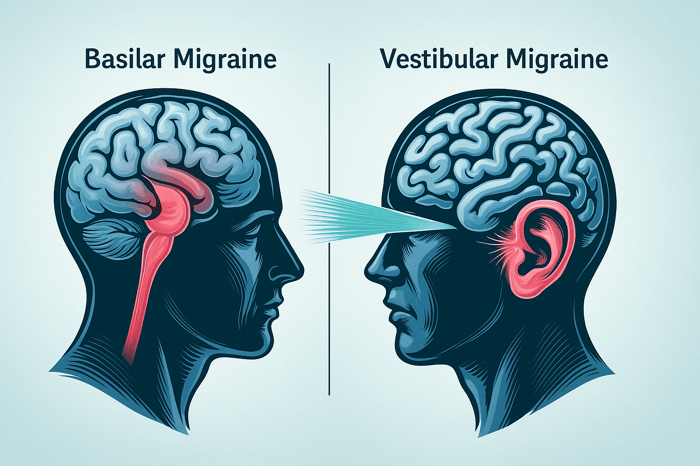
How do different forms of migraine relate to genetic inheritance?
While migraine headaches share a genetic basis, different types of migraine show varying degrees of heritability.
Familial hemiplegic migraine, a rare form with temporary paralysis, has the strongest genetic link with specific gene mutations (CACNA1A, ATP1A2, SCN1A) that can be directly traced through families.
Migraine with aura, characterized by visual disturbances and blind spots, shows higher heritability than migraine without aura.
The genetic associations for episodic migraine differ somewhat from chronic migraine patterns, suggesting that while the neurological disorder has common genetic factors, the expression of these genes varies based on additional environmental and lifestyle factors.
When considering your family's medical history, it's important to note which type of migraine your relatives experience, as this may provide clues about your own risk factors.
If migraines are hereditary, why does their severity vary so dramatically among family members?
The variation in severe headaches among family members with the same genetic variants highlights the complex interplay between genes and environment.
Gene expression in migraine disorders is significantly influenced by environmental factors like stress, diet, and sleep patterns.
Two siblings may inherit similar genetic risk factors for migraine, but the one who experiences more triggers like strong odors, irregular sleep, or blood pressure issues may develop more severe migraine.
Additionally, epigenetic changes, modifications that affect how genes work without changing DNA sequence, can occur throughout life and explain why one family member experiences debilitating head pain while another has only occasional mild episodes.
Research on the genetic basis of migraine suggests that what you inherit is not the migraine itself but rather a predisposition or lowered sensitivity threshold to migraine triggers. The frequency of attacks is then determined by how often environmental conditions, lifestyle choices, or personal triggers push you beyond that threshold.
Can keeping a headache diary help identify if my migraines are hereditary or triggered by environmental factors?
A detailed headache diary is one of the most valuable tools for distinguishing between genetic and environmental influences on your migraine headaches.
By systematically tracking the timing, duration, and intensity of your head pain alongside potential triggers like sensitivity to light, strong odors, or stress, patterns often emerge that weren't previously obvious.
If your migraine occurs regardless of environmental conditions or follows hormonal patterns, genetic components may be more dominant.
Conversely, if clear connections to specific foods, weather changes, or sleep disruptions appear, environmental triggers may be playing a larger role despite any genetic predisposition.
Many people with migraine discover through careful tracking that their condition represents an interaction between their genetic vulnerability and specific major triggers, information that can help tailor better approaches and potentially lower the frequency of attacks through targeted lifestyle modifications.
How does the prevalence of migraine in my family affect my children's risk of developing this neurological disorder?
Families with multiple members experiencing migraine with aura or visual disturbances show stronger genetic transmission than those with migraine without aura.
Gender also plays a role in this genetic puzzle, daughters of mothers with migraine face higher risks than sons, partly due to hormonal interactions with gene expression.
The genetic variants involved typically affect neurotransmitter regulation, ion channel function, and pain processing pathways.
Parents with migraine should know that while they can't change their children's genetic inheritance, early identification of symptoms and proactive management of environmental factors can significantly moderate the development of migraine in genetically predisposed children.
Beyond common gene mutations, what other health conditions might share a genetic link with migraine headaches?
The genetic overlap between migraine and other health conditions provides fascinating insights into the broader implications of migraine-related genes.
Research has identified shared genetic associations between migraine and cardiovascular disorders, with common variants affecting blood vessel regulation and blood flow.
Depression and anxiety also share substantial genetic connections with migraine, explaining why these conditions frequently co-occur.
Less obvious connections exist with certain autoimmune conditions and sleep disorders, suggesting common underlying biological pathways.
Interestingly, some migraine sufferers show genetic variants that affect mitochondrial function, which may explain the comorbidity between migraine and certain metabolic disorders.
Understanding these genetic connections can be valuable for people with migraine when discussing their complete medical history with healthcare providers, as approaches that address these shared genetic factors might help manage multiple conditions simultaneously.
Family members with these related health conditions might also benefit from being aware of their potentially increased migraine risk, even if they haven't experienced severe headaches themselves.
Conclusion
While the question "Are migraines hereditary?" often points to a strong family connection, the story doesn't end there.
Your genetic blueprint, influenced by both nuclear and mitochondrial DNA, certainly sets the stage for migraine susceptibility.
Faulty mitochondria and an energy-deficient brain can make you more vulnerable.
However, understanding this genetic link is empowering, not defeating.
Genes may load the gun, but triggers related to lifestyle, environment, hormones, and metabolism ultimately pull it.
By focusing on strategies that boost mitochondrial function, consistently managing your personal triggers through smart lifestyle choices, and exploring better medical approaches when necessary, you can significantly break the hereditary cycle.
You have the power to influence how your genes express themselves and rewrite your family's migraine narrative, paving the way for fewer attacks and a better quality of life.