At a Glance
|
Understanding the connection between histamine and migraines might unlock a key to managing your headaches more effectively.
Histamine, a chemical involved in immune responses and various bodily functions, can also be a significant player when it comes to migraine triggers.
Many people are unaware of how their diet and lifestyle choices can influence histamine levels in their bodies, which can contribute to headaches and migraines.

Certain foods, stress, and other environmental factors can cause excess histamine release or accumulation, potentially leading to more frequent or severe migraines.
In this article, we will explore the science behind histamine and its relationship with migraines, revealing common triggers and offering actionable strategies to manage symptoms.
By gaining a deeper understanding of how histamine impacts your health, you’ll be better equipped to make lifestyle changes, identify triggers, and seek appropriate treatments.
So, let’s dive into the fascinating world of histamine and see how it can help you take control of your migraine!
Histamine and the Migraine Threshold
Before we go into all the details, we want to give you most practical parts right off the bat.
Histamine intolerance can lower a person's migraine threshold, making them more susceptible to attacks.
Think of your migraine threshold as a bucket - each potential trigger adds to this bucket, and when it overflows, a migraine occurs.
High histamine levels can keep this bucket near its limit, if you are sensitive or intolerant to histamine.
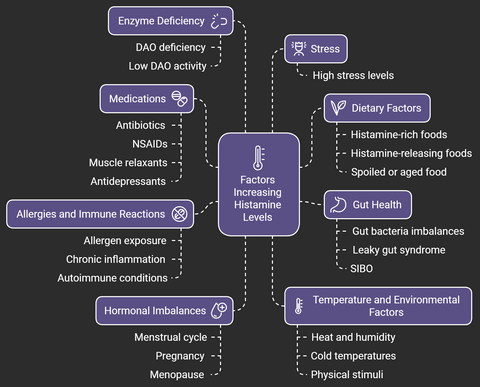
Factors that can increase histamine levels include:
1. Dietary Factors:
- Histamine-rich foods: Certain foods naturally contain high levels of histamine, such as aged cheeses, fermented foods (sauerkraut, kimchi, yogurt), smoked meats, fish, and alcoholic beverages (especially red wine and beer).
- Histamine-releasing foods: Some foods may not contain much histamine but can trigger the body to release histamine, including citrus fruits, tomatoes, strawberries, and certain food additives.
- Spoiled or aged food: As food ages, histamine levels can increase, particularly in protein-rich items like meat and fish.
2. Medications:
- Certain medications can trigger histamine release or inhibit its breakdown. Examples include some antibiotics, NSAIDs (like aspirin and ibuprofen), muscle relaxants, and certain antidepressants.
3. Enzyme Deficiency:
- DAO (Diamine Oxidase) deficiency: DAO is an enzyme responsible for breaking down histamine. A deficiency or low activity of DAO can lead to an accumulation of histamine in the body, causing symptoms.
4. Gut Health:
- Imbalances in gut bacteria or issues such as leaky gut syndrome or SIBO (Small Intestinal Bacterial Overgrowth) can lead to higher histamine production.
- Certain bacteria in the gut produce histamine, so an imbalance in the gut microbiome can contribute to increased histamine levels.
5. Allergies and Immune Reactions:
- Exposure to allergens (pollen, dust mites, pet dander, etc.) can trigger the immune system to release histamine as part of an allergic response.
- Chronic inflammation or autoimmune conditions can also lead to increased histamine production.
6. Stress:
- High stress levels can trigger the release of histamine, as stress affects the immune system and can promote inflammation.
7. Hormonal Imbalances:
- Fluctuations in hormones, such as those that occur during the menstrual cycle, pregnancy, or menopause, can affect histamine levels. Estrogen, for example, can enhance histamine release and inhibit its breakdown.
8. Temperature and Environmental Factors:
- Heat and humidity: Exposure to warm temperatures can stimulate histamine release.
- Cold temperatures or physical stimuli: Conditions like cold urticaria can cause histamine release as a reaction to cold exposure.
Understanding these factors and how they may interact in an individual’s body can be important for managing histamine-related issues, such as migraine.
To reduce your migraine risk, you can:
- Follow a low-histamine diet
- Identify and manage food sensitivities
- Use stress-reduction techniques
- Minimize exposure to oxidative stress factors
Here is nice infographic that will sum up this information:
That being said, let's go into details, enjoy.
Understanding Histamine: The Body's Chemical Messenger
Histamine is a key chemical in our bodies.
It helps control many functions and plays a big role in allergic reactions.
Let's dive into how histamine works and its effects on our health.
Role of Histamine in Body Functions
Histamine helps us sleep, eat, and even feel emotions.
In the stomach, it makes acid. During allergies, it causes symptoms like sneezing and itching.
Its main roles include:
- Immune Response: Histamine is released during allergic reactions to help protect the body by increasing blood flow and inflammation at the site of infection or injury.
- Gastric Acid Secretion: It stimulates the stomach lining to produce gastric acid, aiding in digestion.
- Neurotransmission: Histamine acts as a neurotransmitter in the brain, contributing to alertness and the sleep-wake cycle.
- Regulating Inflammation: It helps regulate local immune responses and inflammation.
While histamine is vital for these functions, excessive levels can lead to symptoms like itching, hives, and other allergic reactions, as well as migraine.
Types of Histamine Receptors
We have four types of histamine receptors in our bodies. Each one has a special job:
- H1 receptors: Control sleep and appetite
- H2 receptors: Manage stomach acid production
- H3 receptors: Linked to brain function and pain perception
- H4 receptors: Involved in immune responses
Mast Cells and Histamine Release
Mast cells are immune cells that store and release histamine.
They're found in skin, nerves, lungs, and intestines. When they're triggered, mast cells release histamine, leading to various reactions in the body.
Knowing about histamine helps us understand many body reactions.
This knowledge is key for managing conditions linked to histamine imbalance, such as migraine.
The Science Behind Histamine Intolerance
Histamine intolerance is officially considered relatively uncommon, but it may be underdiagnosed.
It is estimated that approximately 1-3% of the population may be affected, although true prevalence rates are uncertain due to the challenges in diagnosing the condition.
It is more commonly seen in middle-aged adults, with a higher incidence reported among women.
Histamine intolerance happens when the body can't break down histamine properly.This leads to various symptoms.
The enzyme diamine oxidase (DAO) plays a crucial role in this process, breaking down dietaryhistamine in the gut.
Low DAO levels mean more histamine in the blood.
This can cause a range of problems, from digestive issues to light sensitivity.
Research has found over 50 genetic variations that can affect DAO production, impacting symptoms.
A study found that 92% of people with histamine intolerance experience bloating.
Other common symptoms include skin reactions and headaches, including migraine.
Even healthy people can show symptoms after consuming a meal with histamine.
Symptom | Percentage of Affected Individuals |
Bloating | 92% |
Skin Pruritis | 48% |
Headache/Migraine | Less common than digestive symptoms |
Here is a link to the study for mentioned stats.
There's a strong link between histamine intolerance and migraines.
About 90% of people with severe migraines lack DAO. This shows how important it is to manage histamine levels to prevent migraines.
Common Symptoms of Histamine Overload
Histamine intolerance can cause many symptoms in the body. These are most common symptoms:
- Digestive System Reactions: Gastrointestinal issues are common in histamine overload. Symptoms include bloating, abdominal pain, and changes in bowel movements. People often feel nauseous, vomit, and have too much gas.
- Neurological Manifestations: Dizziness and headaches, including migraines, are often reported. Some may feel anxious or have trouble regulating their body temperature.
- Skin and Respiratory Symptoms: Itchy skin and hives are typical. Respiratory issues like nasal congestion and breathing problems may also occur. Some people experience irregular heart rates and high blood pressure.
Category | Symptoms |
Skin-Related | Hives (urticaria), itching (pruritus), flushing/redness, eczema-like rashes |
Digestive | Abdominal pain, bloating, gas, diarrhea, nausea, vomiting |
Respiratory | Nasal congestion, runny nose (rhinitis), sneezing, difficulty breathing, asthma-like symptoms |
Neurological | Headaches, migraines, dizziness, vertigo, fatigue, anxiety, mood disturbances |
Cardiovascular | Rapid heartbeat (tachycardia), low blood pressure (hypotension) |
Other | Flushing/overheating after histamine-rich foods, menstrual irregularities |
These symptoms can be similar to other conditions like IBS and migraine.
This makes it hard to diagnose. If you have symptoms in different parts of your body, see a healthcare professional for help.
That being said, let's uncover the connection between histamine and migraine, this might surprise you!
The Connection Between Histamine and Migraine
Histamine is key in migraines. Research links high histamine levels to migraine attacks.
People with migraines often have more histamine in their blood than others and in some patients the activity of the histamine digesting enzyme DOA has been shown to be reduced
The trigeminal nerve is important in migraines. Histamine can cause inflammation in this nerve and the meninges.
This inflammation leads to the release of neuropeptides like CGRP, which are vital in migraine development.
Histamine makes blood vessels wider.
This change is thought to cause migraine pain. People with migraines often have allergies and asthma, which are also linked to histamine.
Mast cells release histamine in the meninges when stressed or due to diet.
This release can start a migraine attack.
Factor | Impact on Migraines |
Plasma Histamine Levels | Increased in migraine patients |
Mast Cell Activation | Correlates with migraine progression |
Diamine Oxidase (DAO) Activity | Low levels observed in migraine sufferers |
Histamine-Related Conditions | Higher prevalence in migraine patients |
Understanding this connection opens new ways to manage migraines.
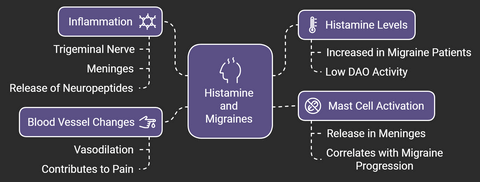
Targeting histamine pathways could lead to better treatments for this condition.
The Role of Diamine Oxidase (DAO) in Migraine Prevention
Diamine oxidase breaks down histamine in our bodies and low DAO levels can cause histamine buildup, which may trigger migraines.
Knowing this helps manage migraine symptoms better.
DAO deficiency happens when the body doesn't make enough of this enzyme. Studies show 87% of migraine patients have low DAO levels.
This can lead to too much histamine, causing severe headaches.
Testing for DAO Levels
It's important to find out if you have DAO deficiency.
The MIGRATEST, by SYNLAB, tests DAO levels in the blood.
This test shows if histamine intolerance is causing your migraines, helping find the right treatment.
Enzyme Supplementation Options
For those with DAO deficiency, supplements can help. A study with 100 migraine patients showed good results.
Those taking DAO supplements saw their migraine time drop from 6.14 to 4.76 hours.
The placebo group didn't see as much improvement. Importantly, DAO supplements had no side effects.
Group | Initial Duration (hours) | Final Duration (hours) | Reduction |
DAO Supplement | 6.14 | 4.76 | Significant |
Placebo | 7.53 | 6.68 | Non-significant |
These results suggest DAO supplements could help prevent and manage migraines.
As research goes on, it might offer new hope for those with histamine-related migraines.
Here is a link to the study with all results.
High-Histamine Foods to Watch Out For
The most common culprits are fermented and aged products, where histamine levels increase over time.
This includes aged cheeses like parmesan and blue cheese, fermented vegetables such as sauerkraut and kimchi, and alcoholic beverages, particularly red wine and beer.
Protein-rich foods can also be problematic, especially when they're not fresh.
Aged or cured meats, leftover proteins, and preserved fish products tend to accumulate higher histamine levels.
Even certain fresh fruits and vegetables might trigger reactions – avocados, eggplant, spinach, tomatoes, strawberries, and citrus fruits are known to be histamine-rich or histamine-liberating foods.
Condiments and seasonings can be unexpected sources of histamine.
Vinegar-based products, soy sauce, fish sauce, and yeast extracts often contain significant amounts.
Even chocolate, a common migraine trigger, contains compounds that can influence histamine levels in the body.
Managing histamine intake requires careful attention to food choices and timing.
Fresh foods generally contain lower histamine levels than preserved or stored foods. Keeping a detailed food diary can help identify personal triggers, as sensitivity varies significantly among individuals.
It's also important to maintain regular eating patterns, as skipping meals can trigger migraines independently of histamine intake.
Working with a healthcare provider to develop a personalized low-histamine diet plan can be particularly beneficial, especially since eliminating too many foods without proper guidance might lead to nutritional deficiencies.
Here are some basic examples of these foods:
Category | High-Histamine Foods | Histamine Level |
Fermented Foods | Sauerkraut, kimchi, pickles, soy sauce, miso, kombucha | Very High |
Aged Cheeses | Cheddar, Parmesan, Gouda, Swiss cheese, blue cheese | Very High |
Processed/Cured Meats | Salami, ham, bacon, sausages, pepperoni | Very High |
Alcoholic Beverages | Red wine, beer, champagne, certain spirits | High |
Smoked/Canned Fish | Tuna, mackerel, sardines, anchovies | Very High |
Vegetables | Spinach, eggplant, avocado, tomatoes | Moderate to High |
Vinegar-Based Foods | Pickled vegetables, vinegar (e.g., ketchup, salad dressings) | High |
Other Foods | Dried fruits (raisins, dates), certain nuts (walnuts, cashews), chocolates, fermented dairy (yogurt, kefir) | Moderate to High |
Fruits | Citrus fruits (oranges, lemons, limes), strawberries, pineapples, bananas | Low (but triggers release) |
Seafood | Certain shellfish | Low to Moderate (but triggers release) |
This table indicates that foods marked as "Very High" or "High" should be approached with caution by individuals with histamine intolerance, while foods that are "Low" may still trigger histamine release without being high in histamine themselves.
Knowing about these foods helps you make a diet plan.
Keeping track of what you eat and how you feel can help find what triggers your migraines. This can help manage them better.
Treatment Approaches for Histamine-Related Migraines
When managing histamine-related migraines, a multi-faceted approach often yields the best results.
The goal is to reduce histamine load while supporting the body's natural ability to process histamine effectively.
Dietary Modifications
The foundation of managing histamine-related migraines starts with diet.
Beyond simply avoiding high-histamine foods, a comprehensive dietary strategy should include eating fresh foods whenever possible, as histamine levels increase in foods over time.
Batch cooking with immediate freezing can help, as freezing pauses histamine development.
Incorporating foods rich in vitamin C, B6, and copper can support the body's natural histamine breakdown processes.
Many find success with a rotation diet, where potentially triggering foods are eaten only every few days to prevent histamine buildup.
Antihistamine Medications
While antihistamines are commonly associated with allergies, they can play a crucial role in managing histamine-related migraines.
H1 blockers like loratadine or fexofenadine may help prevent attacks, while H2 blockers such as famotidine might reduce digestive symptoms that often accompany histamine reactions.
Some neurologists prescribe mast cell stabilizers for severe cases, which help prevent histamine release in the body.
However, medication choices should always be discussed with a healthcare provider, as individual responses vary and some medications may have side effects.
Natural Remedies
Several natural approaches can complement conventional treatments.
Quercetin, a natural antihistamine found in onions and apples, may help stabilize mast cells and reduce histamine release.
Vitamin C not only supports histamine breakdown but also has natural antihistamine properties.
DAO (Diamine Oxidase) enzyme supplements can help break down histamine from foods, particularly when taken before meals. Other beneficial supplements may include:
- Magnesium (helps reduce histamine levels)
- B vitamins (support histamine metabolism)
- Omega-3 fatty acids (reduce inflammation)
- Probiotics (specific strains that don't produce histamine)
Additional supportive measures include:
- Stress management techniques
- Regular gentle exercise
- Adequate sleep
- Proper hydration
- Temperature management (avoiding excessive heat)
Success in managing histamine-related migraines often requires a personalized combination of these approaches, fine-tuned over time with professional guidance.
Keeping a detailed symptom journal can help identify which treatments work best for individual cases.
Remember, what works for one person may not work for another, and it often takes time to find the right combination of treatments.
Here's a short comparison of treatment strategies:
Approach | Effectiveness | Side Effects | Accessibility |
Low-Histamine Diet | High – Reduces histamine intake | Minimal, possible nutritional limitations | Easy, requires dietary planning |
Fresh Food Consumption | High – Prevents histamine buildup | None | Very accessible |
Avoid Histamine Liberators | Moderate – Reduces histamine release | Minimal | Easy |
DAO Enzyme Supplements | Moderate to High – Breaks down histamine | Possible mild digestive discomfort | Moderate, available over-the-counter |
Vitamin C & B6, Magnesium, Omega 3 | Moderate – Supports DAO and lowers histamine & inflammation | Minimal | High, widely available |
Quercetin | Moderate – Stabilizes mast cells | Rare allergic reactions | Moderate, available as supplements |
H1 and H2 Antihistamines | High – Reduces symptoms effectively | Drowsiness, dry mouth, dizziness | High, prescription/over-the-counter |
Stress Management | Moderate – Reduces histamine triggers | None | Very accessible |
Good Sleep Hygiene | Moderate – Supports immune function | None | Very accessible |
Avoid Certain Medications | Moderate – Prevents histamine increase | Depends on alternative medications | Requires medical advice |
Testing for DAO Levels | High – Identifies histamine intolerance | None | Moderate, requires medical support |
Addressing Underlying Conditions | High – Reduces chronic symptoms | Depends on treatment | Medical consultation needed |
Selective Probiotics | Moderate – Supports gut health | Minimal | Moderate, available in health stores |
What works best can differ from person to person. Always talk to a healthcare professional to create a treatment plan that's right for you.
Frequently Asked Questions
You might find yourself with additional questions regarding the relationship between histamine intolerance and migraine.
To help address a variety of these questions—from basic to more complicated—we’ve prepared a list of frequently asked questions for you.
Here are insightful FAQs about histamine and migraines incorporating your requested keywords:
Can seasonal allergies increase the frequency of migraines through heightened histamine release?
Yes, seasonal allergies can trigger increased release of histamine, potentially leading to more frequent migraines.
During allergy seasons, the body's elevated inflammatory response and histamine levels can make individuals more susceptible to migraine attacks, especially if they already have a sensitivity to histamine.
How do endothelial cells respond to high levels of histamine during a migraine attack?
Endothelial cells lining blood vessels react to elevated histamine levels by dilating, which can lead to inflammation and increased permeability of the blood-brain barrier.
This process can contribute to both the pain and sensitivity to light commonly experienced during migraines.
Is there a connection between histamine intolerance and weight gain in migraine sufferers?
Yes, histamine intolerance can indirectly contribute to weight gain in migraine patients.
The inflammatory response triggered by excess histamine can affect metabolism and lead to fluid retention. Additionally, some medications used in migraine treatment may impact weight management.
How does the basal ganglia's response to histamine influence the migraine process?
The basal ganglia, a key brain region involved in pain processing, contains numerous histamine receptors.
When exposed to high levels of histamine, it can modify pain perception and contribute to the complex neurological cascade that characterizes the migraine process.
Can a stuffy nose be an early warning sign of a histamine-triggered migraine?
Yes, nasal congestion can be a prodromal symptom of a histamine-related migraine. The allergic response causing the stuffy nose often indicates elevated histamine levels, which may precede a full migraine attack by several hours.
How do elimination diets differ from standard low-dietary histamine approaches in migraine treatment?
While low-dietary histamine approaches focus specifically on reducing histamine-rich foods, elimination diets systematically remove and reintroduce various dietary triggers to identify personal sensitivities.
This broader approach helps pinpoint whether histamine or other compounds are the primary triggers for an individual's migraines.
Is there a correlation between migraine severity and the dose of histamine in the body?
Research suggests a direct correlation between migraine intensity and histamine levels, with higher doses of histamine typically associated with more severe symptoms and longer duration of attacks. However, individual sensitivity varies significantly.
How do cluster headaches differ from histamine-induced migraines in terms of treatment approach?
While cluster headaches and histamine-induced migraines may share some symptoms, their treatment approaches differ.
Cluster headaches often require specific acute interventions, whereas histamine-induced migraines may respond better to preventive measures focusing on histamine management and dietary modifications.
Conclusion
Understanding the connection between histamine and migraines can help you manage and reduce headache frequency.
Histamine can trigger migraines by causing inflammation and widening blood vessels, often linked to food, stress, and other factors.
To manage this, focus on dietary changes, such as avoiding high-histamine foods, and consider supplements like DAO to help break down histamine.
Antihistamines and natural remedies can also offer relief. A combination of lifestyle changes, medical treatments, and personal strategies, tailored to your needs, can significantly improve migraine control and quality of life.