At a Glance
|
As flu season gets closer, people with migraine face a big challenge.
They must deal with flu symptoms and prevent migraine attacks, which can increase during an infection..
The flu and migraine can make each other worse, especially with symptoms like body aches and fever.

Headaches often start soon after getting the flu. Increased inflammation, oxidative stress, dehydration from fever and sinus pressure all can cause headaches.
Stress and lack of sleep can also lead to tension headaches.
Many of the mechanisms that come with a flu or the immune response to the invader, can also contribute to migraine, making this worse for those migraine sufferers.
With the right tips and strategies, people may get through the flu season easier.
They can also help lessen the effects of flu and migraine on their daily lives.
Understand the Impact of Flu If You're a Migraine Sufferer
The flu can trigger migraines due to a combination of different factors, such as the immune response, metabolic changes, and oxidative stress.
Inflammatory and Immune Response
During a flu infection, the immune system releases pro-inflammatory molecules like cytokines and interleukins.
These molecules lead to inflammation and alter pain pathways, making the body more sensitive to pain, especially in migraine-prone individuals.
This inflammatory response can lead to heightened trigeminal nerve sensitivity, which is closely related to migraine onset.
Metabolic Stress
Fighting off the flu places metabolic stress on the body, requiring a higher-than-normal energy expenditure to produce immune cells and proteins.
This can deplete energy reserves in the body. Such energy demands strain the brain's supply, which is crucial for normal function.
The resulting energy deficiency, especially in a brain that may already be sensitive to metabolic changes, can serve as a trigger for migraines.
In addition, fatigue and low energy due to this metabolic stress can make the brain more vulnerable to migraine.
Oxidative Stress
Flu infections increase the production of reactive oxygen species (ROS) as the immune system attacks viral particles with exactly these ROS bombs, which are also harmful for our own cells.
While ROS helps fight infection, high levels of oxidative stress can damage cells and lead to neuroinflammation.
In migraine patients, this oxidative stress can overwhelm the brain’s antioxidant defenses (e.g., glutathione), increasing the likelihood of triggering a migraine.
Moreover, oxidative stress can disturb the balance of ions like calcium and potassium, affecting neural function and making the brain more prone to migraine.
Hormonal and Neurotransmitter Imbalances
Infection-related inflammation can disrupt serotonin levels and other neurotransmitters like dopamine, which play a role in migraines.
Reduced serotonin during infection can lower the threshold for migraine, as serotonin is known to regulate pain and mood.
In summary, the combination of inflammation, metabolic and oxidative stress, and neurotransmitter changes due to the flu creates an environment that can easily trigger migraines, especially in those with a predisposition to them.
Managing oxidative stress with antioxidants and maintaining hydration can help mitigate some of these effects.
Flue Trigger Factor | Mechanism | Impact on Migraine |
Inflammatory Response | Release of cytokines and interleukins increases inflammation and pain sensitivity. | Heightens trigeminal nerve sensitivity, triggering migraine. |
Metabolic Stress | High energy demand depletes glucose, increases lactate, causing energy imbalance. | Brain vulnerability to migraine due to low energy reserves. |
Oxidative Stress | Immune response generates ROS, leading to neuroinflammation and ion imbalance. | Exacerbates neural sensitivity, increasing migraine risk. |
Hormonal Imbalance | Flu-related inflammation can disrupt serotonin and other neurotransmitters. | Lower serotonin threshold makes migraines more likely. |
Common Flu Symptoms That Exacerbate Migraine
It's important to know the signs of the flu, especially if you get migraine.
The flu can make migraine worse, creating a tough cycle to break.
Knowing these symptoms helps manage migraine better during the flu season.
Identifying Symptoms: Flu versus Allergies
Flu and allergies share some symptoms, which can make it hard to tell them apart.
Symptoms like nasal congestion, and sometimes sore throat, and tiredness often overlap. Both can cause sinus headaches due to pressure in the sinuses.
Allergies can make breathing harder, which can make migraine worse. People with both flu and allergies often find it hard to manage their symptoms.
The immune response to both can contribute to triggering a migraine..
While the flu and allergies share some overlapping symptoms, they also have key differences.
With the flu, fever, body aches, fatigue, and a dry cough are common, often accompanied by a sore throat. Flu symptoms usually last 1–2 weeks and can be quite intense.
Allergies, on the other hand, rarely cause fever or body aches. Instead, they often lead to itchy eyes, a runny or stuffy nose, and sometimes a cough due to post-nasal drip.
Allergy symptoms persist as long as the person is exposed to allergens, like pollen or dust.
In short, fever and body aches suggest flu, while itchy eyes and prolonged symptoms lean towards allergies, but both can trigger migraine.
Link Between Sinus Infections and Migraine
Many people get sinus infections from the flu. The inflammation from these infections causes intense pressure in the sinuses.
This pressure can feel a bit like migraine pain, but there are many differences as well.
With a sinus infection, common symptoms include facial pressure, pain around the forehead, eyes, or cheeks, nasal congestion and a runny nose.
The pain typically intensifies when bending forward, and you might also experience fatigue and thick nasal discharge. Sinus infections usually last from several days to a few weeks.
In contrast, a migraine is usually marked by intense, throbbing pain on one side of the head, sensitivity to light and sound, nausea, and sometimes visual disturbances (known as auras).
Migraines typically don’t cause nasal congestion or fever and can last from a few hours to several days if untreated.

In short, sinus infections are characterized by congestion and facial pain, while migraines are more associated with throbbing head pain, nausea, and sensitivity to light or sound.
It is important to treat sinus infections quickly, especially if you also suffer from migraine.
Untreated infections can lead to more pain and health problems.
Symptom | Flu | Allergies | Sinus Infections |
Nasal Congestion | Common | Common | Common |
Sore Throat | Common | Occasional | Less Common |
Fatigue | Severe | Mild | Moderate |
Headaches | Common | Occasional | Common |
Facial Pain | Less Common | Less Common | Common |
Managing Sinus Pressure and Migraine Pain
Sinus pressure can really hurt, especially during flu season when a sinus infection is to blame, and can make migraine pain worse.
There are many ways to manage sinus pressure and sinus infection.
Using home remedies is key to feeling better and keeping your sinuses working right.
Effective Home Remedies for Sinus Pain
There are many home remedies for sinus pain. Inhaling steam helps loosen mucus and improve drainage.
Warm compresses on your face can make tenderness and congestion feel better.
Drinking plenty of mineral water or tea or broth is also important to thin mucus and help it drain.
- Inhale steam from hot water containing anti-inflammatory herbs like sage l to ease congestion.
- Apply warm compresses to the forehead and cheeks for pain relief.
- Stay hydrated with warm fluids like herbal tea or broth.
- Utilize a humidifier to add moisture to the air, preventing dryness.
- Rest, nothing helps healing better.
Utilizing Nasal Saline and Steam Inhalation
Nasal saline solutions are great for managing sinus pressure.
Using a saline nasal spray or rinse can clear your nasal passages and ease sinus pain.
This method works well with steam inhalation to remove mucus and reduce swelling.
Method | Benefit |
Steam Inhalation | Loosens mucus and promotes drainage |
Warm Compress | Reduces tenderness and pain |
Nasal Saline | Cleanses nasal passages and reduces pressure |
Hydration | Thin mucus and eases sinus congestion |
Utilizing Pain Relievers and Counter Medications During Flu Season
Managing migraine during flu season often requires effective pain relievers.
Many individuals turn to over-the-counter medication for relief, especially when flu symptoms overlap.
It's important to know how and when to use these medications to manage flu or migraine symptoms well.
When to Use Over-the-Counter Pain Relievers
Over-the-counter pain relievers can help treat acute migraine or flu related headache symptoms.
Acetaminophen and NSAIDs, like ibuprofen and naproxen, are popular choices. Acetaminophen is in over 600 products and is often recommended first for those who can't take NSAIDs.
Dosages should never exceed 4,000 milligrams per day to avoid liver damage.
Liver damage is a leading cause of acute liver failure in the U.S.
Some effective options for acute severe headache treatment include:
- Acetaminophen: Can alleviate mild to moderate migraine pain.
- Ibuprofen: Shown to provide relief during migraine attacks for about half the population.
- Naproxen: Found to be superior to a placebo for easing migraine pain.
- Aspirin: Doses between 900 and 1,000 mg may help with acute migraine relief.
- Combination products: Using aspirin, acetaminophen, and caffeine together can enhance effectiveness beyond single agents.
Consulting a Healthcare Professional for Severe Headaches
For migraine that is unusually severe or don't respond to over-the-counter medication, seeing a healthcare professional is crucial.
Medication overuse headaches can result from taking pain relievers more than three times per week.
Medical professionals can suggest alternative treatments, including prescription options like triptans or ergot derivatives, which target migraine pain specifically.
Early intervention can prevent further complications and lead to more effective migraine management.
Medication Type | Common Brands | Primary Use | Risks |
Acetaminophen | Tylenol | General pain relief | Liver damage if overused |
NSAIDs | Advil, Aleve, Bayer | Inflammation and pain relief | Risk for ulcers; stomach bleeding |
Combination products | Excedrin | Acute migraine relief | Potential for rebound headaches |
Opioids | Codeine | Severe pain | Addiction; overdose risk |
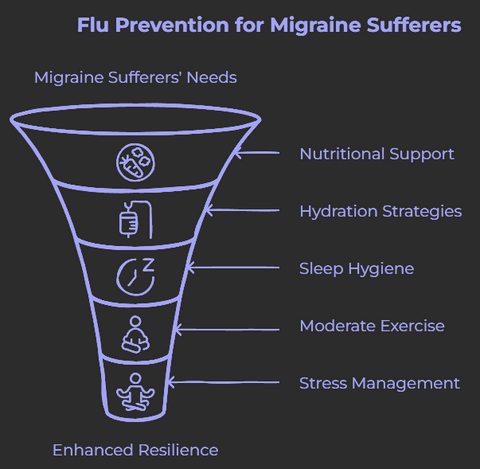
Tips & Strategies for Flu Prevention for Migraine Sufferers
Managing migraine during flu season can be challenging, as the flu can trigger or exacerbate migraine through inflammation, oxidative stress, dehydration, congestion, and metabolic stress.
For those prone to migraine, flu prevention becomes doubly important.
Here’s a guide to flu suppression tailored specifically for migraine sufferers, along with how micronutrients, such as contained in Brain Ritual®, can play a role in boosting resilience during flu season.
Prioritize Quality Sleep
Sleep is vital for both immune and migraine health.
During flu season, prioritizing rest can help prevent both illness and migraine.
- Establish a Consistent Sleep Schedule: A regular sleep routine supports immune resilience and reduces migraine frequency.
- Create a Calming Bedtime Routine: Avoid stimulants like caffeine or screens before bed. Incorporate relaxing activities like reading or meditation, both of which lower stress—a common migraine trigger.
- Create a Sleep Friendly Environment: This means, cool, quiet and dark, qualities also appreciated by the migraine brain.
Stay Hydrated with Migraine-Friendly Fluids
Hydration is key to preventing both flu symptoms and migraine.
Migraine sufferers are particularly sensitive to dehydration, making consistent hydration crucial.
- Opt for Electrolyte-Rich Drinks: Herbal teas and mineral waters help maintain fluid balance.
- Avoid Sugary and Caffeinated Beverages: These can contribute to dehydration. Herbal teas, mineral water, or low-sugar sports drinks are better choices for migraine management.
Focus on Immune-Boosting Nutrition
Nutrition plays a significant role in both flu prevention and migraine management. Adding immune-supporting foods can enhance overall health and reduce flu vulnerability.
- Incorporate Anti-Inflammatory Foods: Omega-3s (found in salmon, walnuts, and flaxseeds) and magnesium-rich foods (like spinach and quinoa) help manage inflammation and migraine triggers.
- Avoid Known Migraine Triggers: Processed foods, foods high in sugar, alcohol, and aged cheeses can trigger migraine and weaken the immune system.
How Brain Ritual® Supports Migraine Management and Immune Health During Flu Season
Brain Ritual® is designed to nourish the brain with essential nutrients, enhancing energy metabolism, and performance, which can be especially beneficial during flu season when migraine sufferers are more vulnerable. It additionally contains nutrients that support the immune system.
Here’s how Brain Ritual® can help:
- Supports Brain Energy Levels: Brain Ritual® provides ketone bodies, an alternative energy source to glucose, to keep brain energy stable. This helps manage migraine symptoms linked to low energy availability, a common issue for migraine sufferers.
- Boosts Immune-Strengthening Nutrients: With a rich blend of vitamins and minerals like zinc, vitamin C, lysine, magnesium, B vitamins, and CoQ10, Brain Ritual® supports the immune system, adding resilience to fight off flu season infections.
- Provides Antioxidant Protection: Ingredients like CoQ10 and vitamin C and E protect brain cells from oxidative stress, which can be heightened during illness. This added antioxidant layer can make the brain less susceptible to migraine triggers exacerbated by flu symptoms.
By combining these benefits, Brain Ritual® not only supports energy metabolism but also may help migraine sufferers maintain a robust immune response during flu season.
In case you want to learn more about Brain Ritual® and the science behind it, you can click here.
That being said, we will go over some very common (and often overlooked) strategies for flu suppression especially if you also suffer from migraine issues.
Strengthen Your Immune System with Moderate Exercise
Moderate exercise, such as walking or yoga, can boost immunity and lower migraine frequency.
Exercise enhances circulation and helps the body fight off infections, but it’s important to avoid high-intensity workouts that might trigger migraine.
- Engage in Low-Intensity Activities: Opt for gentle exercises that avoid the risk of migraine, such as stretching or light yoga.
- Get Outside Safely: Fresh air can improve mood and boost immunity; be sure to bundle up in cooler weather.
Practice Good Hygiene
Basic hygiene practices are essential for flu prevention, particularly for those with migraine, as they may already be managing a sensitive immune system.
- Wash Hands Regularly: Regular handwashing reduces exposure to germs.
- Limit Face-Touching: Avoid touching your face, as flu viruses often enter through the eyes, nose, and mouth.
- Consider Wearing a Mask: In crowded spaces, such as subways, trains, buses or similar, a mask can provide an added layer of flu protection.
Manage Stress to Support Immune Health
Stress reduction is critical for migraine sufferers as stress is a common trigger that also weakens the immune system, making it easier to contract flu.
- Incorporate Daily Stress Management Techniques: Meditation, deep breathing exercises, and mindfulness are effective ways to manage stress and potentially reduce migraine frequency.
- Practice Cognitive Behavioral Therapy (CBT): For those with chronic migraine, CBT can offer valuable coping strategies, improving mental resilience during high-stress flu seasons.
- Learn To Say No: Being a perfectionist or wanting to please everyone can be very stressful and hence overcoming both can be quite effective.
- Get Rid of Toxic Relationships: Whenever possible, chose to spend your valuable time with people that make you feel good, understand you and do not create more stress in your life.
Avoid Medications That May Trigger Migraine
Certain cold and flu medications contain ingredients that can trigger migraine.
Read labels carefully and opt for natural remedies when possible.
- Use Natural Decongestants: Saline sprays, steam inhalation, and essential oils like eucalyptus can help relieve sinus congestion without triggering migraine.
- Consider Migraine-Safe Medications: Talk to a healthcare provider about flu treatments that are compatible with migraine management.
By combining these flu prevention strategies with effective migraine management practices and leveraging the support of products like Brain Ritual®, migraine sufferers can hopefully navigate flu season with greater resilience and fewer triggers.
Taking proactive steps to strengthen both the immune and nervous systems can lead to a healthier, more balanced flu season.
When to Seek Medical Care for Flu and Migraine Symptoms
Some signs mean you need to see a doctor right away, especially during flu season.
Spotting these signs early can stop problems from getting worse and get you the right care fast.
People with severe headaches should watch out for these warning signs:
- Headaches that are sudden and severe, described as the worst headache of your life.
- Persistent headaches that do not improve with over-the-counter medications.
- Headaches accompanied by neurological symptoms such as confusion, difficulty understanding speech, numbness, weakness, or paralysis.
- High fever exceeding 102°F during flu season, particularly in combination with severe headaches.
- Experiencing symptoms like difficulty breathing, severe chest or stomach pain, or dehydration.
Seeing a doctor is a good idea if your headaches are getting worse or more frequent.
If headaches keep you from doing daily activities or sleeping well, it's time to see a doctor.
Not every headache needs emergency care, but knowing the signs can help you get the right treatment quickly.
Frequently Asked Questions
After understanding the various aspects of managing migraine symptoms during flu season, you may still have some questions.
In this section, we've compiled answers to common questions that can help you better navigate this situation.
How can the flu virus exacerbate migraine headaches?
The flu can worsen migraine symptoms by causing inflammation, oxidative stress and metabolic imbalances all of which can lead to increased migraine pain.
Additionally, flu symptoms like fever, body aches, and fatigue can act as triggers for those prone to chronic migraine.
What are the common symptoms that overlap between the flu and migraine?
Both the flu and migraine can cause symptoms like stuffy nose, headaches, and sensitivity to light, sound, and smells.
Distinguishing between the two can be challenging, as sinus pressure from the flu can also trigger migraine attacks.
How can sinus infections resulting from the flu lead to more severe migraine episodes?
The inflammation and pressure build-up in the sinuses due to sinus infections from the flu can directly contribute to the intense facial pain and throbbing associated with migraine. Prompt treatment of sinus infections is crucial for migraine sufferers.
What are some effective home remedies for managing sinus pressure and migraine pain during the flu?
Inhaling steam, sage infusions, using warm compresses, staying hydrated, and utilizing nasal saline sprays can all help provide relief from sinus-related migraine pain. These methods can help reduce inflammation and improve drainage.
When should migraine sufferers consider seeking medical care for flu and headache symptoms?
It's important to see a doctor if headaches are sudden and severe, do not improve with over-the-counter medications, or are accompanied by neurological symptoms like confusion, numbness, or paralysis. High fevers during flu season also warrant medical attention.
How can stress and sleep deprivation from the flu impact migraine frequency?
The flu can disrupt sleep patterns and increase stress, both of which are common migraine triggers.
Establishing a consistent sleep schedule and incorporating stress management techniques can be crucial for migraine sufferers during flu season.
How can the immune-boosting benefits of moderate exercise help mitigate the impact of the flu on migraine?
Light physical activity, such as gentle yoga or walking, can enhance circulation and strengthen the immune system, which may help prevent flu infections and reduce the frequency of migraine episodes.
However, it's crucial to avoid high-intensity workouts that could potentially trigger migraine.
What role can hydration play in managing both flu symptoms and migraine?
Proper hydration is key, as dehydration can exacerbate both flu symptoms and migraine attacks.
Opting for electrolyte-rich drinks and avoiding sugary or caffeinated beverages can help maintain fluid balance and reduce the risk of migraine during the flu season.
Conclusion
Flu season can be tough for people with migraine, but you can take steps to make it easier.
Understanding how the flu can trigger or worsen migraine is essential, and recognizing overlapping signs helps you manage your health effectively.
Prioritize quality sleep, stay hydrated, and use home remedies to ease symptoms.
Preventive measures like immune boosting food, nutrients and supportive products, such as Brain Ritual®, can enhance your resilience during this time.
Always listen to your body; if symptoms worsen, consult your healthcare provider.
By taking proactive steps, you can ensure that flu season remains manageable and less burdensome.




