If you're among the millions of women who experience migraine and need birth control, you've probably wondered if there's a connection between the two, and you'd be right to ask.
Finding the right birth control options for migraine sufferers can feel like navigating a maze, especially when you've heard conflicting information about safety risks.
"Will birth control make my migraine worse?"
"I get aura with my migraine, can I still use hormonal contraception?"
"Are there birth control methods that might actually help my headaches?"
These questions deserve clear answers, because the relationship between migraine and contraception isn't just about comfort, it's about safety too.

Some birth control methods can increase health risks for certain migraine sufferers, while others might offer support from your monthly headache pattern.
In this article, we'll walk through everything you need to know about choosing contraception when you have a migraine.
From understanding the science behind hormone-related headaches to exploring safe, good options that won't worsen your symptoms, we've got you covered.
Hormonal Birth Control and Migraine Can Be a Risky Mix
In this section, we'll explore the complex relationship between hormonal contraceptives and migraine headaches.
For many women with migraine, particularly those with aura, certain hormonal birth control methods may increase stroke risk and they also increase oxidative stress, which is a common denominator of most migraine triggers.
The Pill and Oxidative Stress
The birth control pill can increase something called oxidative stress, which happens when harmful molecules called free radicals build up in the body.
These free radicals can damage cells and reduce the brain’s energy supply by making it harder for the body’s "energy factories" (called mitochondria) to work properly.
Since the brain needs a lot of steady energy, this can make people more likely to get migraines.
Oxidative stress can also trigger inflammation and affect blood flow in the brain, both of which are known to make migraines worse.
Why artificial forms of hormones can make migraine worse
If you've ever noticed your migraine getting worse around your period, you're not imagining things.
The culprit? Estrogen fluctuations. When estrogen levels drop just before your period starts, it can trigger what doctors call "menstrual migraine."
Some pills contain artificial forms of estrogen and this can mess with the body’s own production of estrogen. This is why some birth control methods can be problematic for migraine sufferers.
Combined hormonal contraceptives (CHCs) contain synthetic versions of both estrogen and progestin.
These pills, patches, and rings work well for pregnancy avoidance, but can sometimes throw your migraine patterns into chaos.
The hormonal roller coaster that happens during your natural cycle can be disrupted, sometimes for better, sometimes for worse, when you introduce artificial hormones into the mix.
The danger of using birth control if you have aura
Here's where things get serious: if you experience migraine with aura (those visual disturbances like zigzag lines, blind spots, or flashing lights before your headache hits), you should be especially cautious about estrogen-containing birth control.
Research has shown that the combination of migraine with aura plus estrogen-containing contraceptives significantly increases your risk of ischemic stroke.
This isn't a small concern, medical organizations worldwide advise against using combined hormonal contraceptives if you have migraine with aura, regardless of your age.
The increased stroke risk simply isn't worth it, especially when safer alternatives exist.
Even if you have migraine without aura, you'll want to be careful with combined hormonal contraceptives if you're over 35 or have other risk factors like smoking or high blood pressure, as these can further increase cardiovascular risks.
When hormonal birth control might actually help
It's not all bad news! Some women with migraine without aura actually experience fewer headaches on certain hormonal birth control regimens.
By maintaining more stable hormone levels throughout your cycle, some birth control methods can suppress the estrogen "crash" that triggers menstrual migraine.
Extended or continuous-use birth control pills (where you skip the placebo pills and take active pills all month) can eliminate withdrawal bleeds and the hormonal fluctuations that come with them.
For some women, this approach minimizes migraine frequency. The question is only at which price and for how long.
However, this approach is generally only considered for women without aura who have no additional cardiovascular risk factors.
Safe Birth Control Options That Don't Worsen Migraine
After reading the previous section, you might be wondering what birth control options are actually safe if you suffer from migraine.
Fortunately, several methods don't increase your risk of stroke or worsen migraine symptoms.
Progestin-only methods that avoid estrogen risks
For migraine sufferers, especially those with aura, progestin-only methods may offer decent contraception without the stroke risks associated with estrogen. These options include:
The "mini-pill," which contains only progestin and must be taken at the same time each day for maximum impact.
While it requires more consistent use than combined pills, it eliminates estrogen-related risks.
Long-acting methods like the hormonal IUD (such as Mirena or Kyleena), which releases small amounts of progestin locally in your uterus rather than throughout your bloodstream.
These IUDs can last 3-8 years depending on the type and often minimize menstrual bleeding and associated hormone fluctuations.
The implant (Nexplanon), a tiny rod inserted under the skin of your arm that releases progestin for up to 5 years, provides good contraception without estrogen.
Depo-Provera, a progestin injection given every three months, which can sometimes help with migraine by suppressing your natural cycle.
However, some women report headaches as a side effect, so results vary person to person.
These options may not elevate stroke risk as much, but they still raise oxidative stress and will add an artificial source of a hormone that may interfere with your own bioidentical progesterone production, so they still come at a price.
In the long run, even these contraceptive pills or hormonal contraceptives can raise your migraine risk and threshold.
How non-hormonal IUDs protect without side effects
The copper IUD (Paragard) stands out as an excellent option for migraine sufferers who want to avoid hormones altogether.
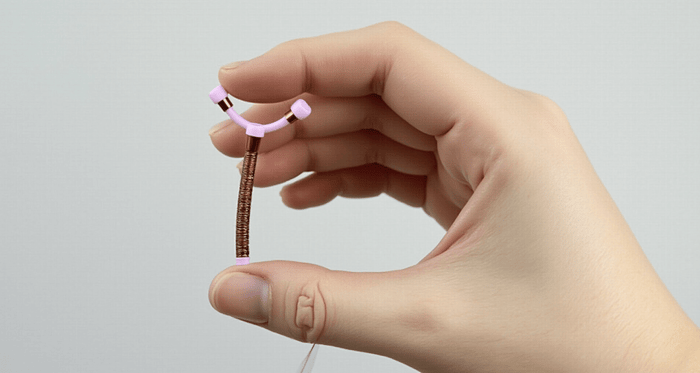
This small T-shaped device works differently than hormonal methods, the copper creates an environment that's toxic to sperm while also making the uterine lining less receptive to implantation.
With no hormones to trigger migraine or increase stroke risk, the copper IUD can be safe for women with any type of migraine.
It's also great (over 99% effect) and can remain in place for up to 12 years, making it both convenient and cost-effective long-term.
The main downside? Some women experience heavier periods or more cramping, especially in the first few months after insertion.
A copper coil does create a local inflammation that can be bothersome and even have a migraine effect for some over time, however, many tolerate it fine.
Formigraine sufferers looking for reliable, non-hormonal protection, these trade-offs often seem minor compared to the potential risks of hormonal methods.
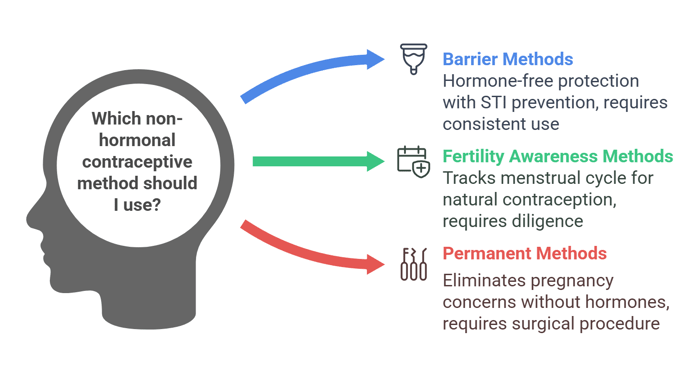
Barrier and fertility-based methods as migraine-friendly choices
If you're looking for the best options with absolutely no systemic effects, barrier methods like condoms, diaphragms, cervical caps, and sponges offer hormone-free protection without affecting your migraine patterns.
Male condoms have the added benefit of protecting against sexually transmitted infections, but they require consistent use with every act of intercourse.
Fertility awareness methods (FAMs) involve tracking your menstrual cycle through various signs like basal body temperature, cervical mucus changes, and cycle length to identify fertile days when you should abstain or use backup contraception.
Modern FAM approaches can be quite good when practiced diligently, and apps and tracking devices have made them more accessible than ever.
For those completely certain they don't want children (or more children), permanent methods like tubal ligation for women or vasectomy for men eliminate pregnancy concerns without affecting hormone levels or migraine patterns.
These surgical procedures provide permanent contraception with no ongoing maintenance required.
To sum this up, here’s a summary of safe birth control options for migraine sufferers:
Method Type | Specific Options | Benefits | Considerations | Safety for Migraine with Aura |
Progestin-Only | Mini-pill | No stroke risk from estrogen | Must take at same time daily | Maybe safe, but long-term risk is still there |
Hormonal IUD (Mirena, Kyleena) | Local hormone release, 3-8 years duration | Insertion procedure required | Maybe safe, but long-term risk is still there | |
Implant (Nexplanon) | Good for up to 5 years | Minor insertion procedure | Maybe safe, but long-term risk is still there | |
Depo-Provera injection | Every 3 months, may minimize menstrual migraine | Some report headaches as side effect | Maybe safe, but long-term risk is still there | |
Non-Hormonal | Copper IUD (Paragard) | No hormones, good for up to 12 years | May increase bleeding/cramping | Probably safe |
Barrier Methods | Condoms, diaphragms, cervical caps, sponges | No hormones, no systemic effects | Requires consistent use, risk of breakage must be considered | Safest |
Fertility Awareness | Tracking fertile days | Hormone-free, increased body awareness | Requires diligent tracking, irregular cycles may pose a challenge | Safest |
Permanent | Tubal ligation, vasectomy | One-time procedure, permanent | Not easily reversible or not at all reversible | Generally safe |
Choosing the Right Birth Control When You Get Migraine
Selecting the appropriate birth control method when you suffer from migraine requires careful consideration of your specific migraine type, overall health, and lifestyle preferences.
This section provides guidance on navigating this important decision with your healthcare provider.
Consulting with your doctor
If you experience migraine, especially with aura, your conversation with healthcare providers should center on safety first. Be prepared to:
Describe your migraine symptoms in detail, particularly any aura experiences
Ask specifically: "Given my migraine type, which contraceptive options pose the lowest risk?"
Discuss warning signs to watch for with any new birth control method
Review additional risk factors like smoking, high blood pressure, or family history of stroke
Consider requesting a referral to a headache specialist or neurologist if your doctor seems uncertain about migraine-contraception interactions
Here are birth control options based on migraine type:
Migraine Type | Recommended Options | Options to Avoid | Why |
With Aura | Best: • Copper IUD • Barrier methods • Sterilization Maybe - Progestin-only pills • Hormonal IUD • Implant (Nexplanon) | Combined hormonal contraceptives (pills, patch, ring) | Estrogen combined with migraine with aura significantly increases stroke risk |
Without Aura (Under 35) | Best: • Copper IUD • Barrier methods • Sterilization Maybe - Progestin-only pills • Hormonal IUD • Implant (Nexplanon • Low-dose estrogen combined pills •Extended/continuous regimens | High-dose estrogen formulations | Lower estrogen doses may minimize migraine triggers while offering additional benefits |
Without Aura (Over 35) | • Progestin-only methods • Non-hormonal methods | Combined hormonal contraceptives | Age plus migraine increases cardiovascular risks with estrogen |
Tracking birth control effects on your migraines
Monitoring how contraceptives affect your migraine patterns is crucial for finding the right method:
Keep a detailed migraine diary tracking:
Frequency, intensity, and duration of attacks
Relationship to your menstrual cycle or birth control schedule
Potential triggers (stress, foods, sleep disruption)
Use technology to your advantage with migraine tracking apps that generate shareable reports for your healthcare provider
Give new methods adequate trial time (typically three months) unless you experience severe side effects or new aura symptoms, which warrant immediate medical attention
Switching methods safely to minimize migraine triggers
Transitioning between contraceptive methods can sometimes trigger hormone-related migraine, but strategic planning helps minimize this risk:
Time your switch carefully - ideally at the end of a pill pack or just after removing a patch or ring
Have a migraine management plan ready including your regular medications, stress minimization techniques, and consistent sleep schedule
Consider different approaches during the transition if you're particularly sensitive to hormonal changes
Maintain open communication with your healthcare provider about any changes in your migraine patterns
Finding the ideal birth control method often requires patience and collaboration with your healthcare team.
The right approach balances good contraception while protecting your neurological health and quality of life.
Complementary Approaches for Migraine Management Beyond Birth Control
While choosing the right contraceptive is crucial for migraine sufferers, many women benefit from a multi-faceted approach to managing their headaches. Options such as red light therapy for migraines and physical therapy exercises for migraines may support neurological recovery in a non-pharmaceutical way.
One innovative option worth considering alongside your birth control choice is medical food specifically designed for migraine management.
Brain Ritual represents an emerging category called medical food that targets the metabolic roots of migraine.
Unlike medications that mask symptoms, medical foods like Brain Ritual address a potential underlying cause: dysfunctional brain energy metabolism.
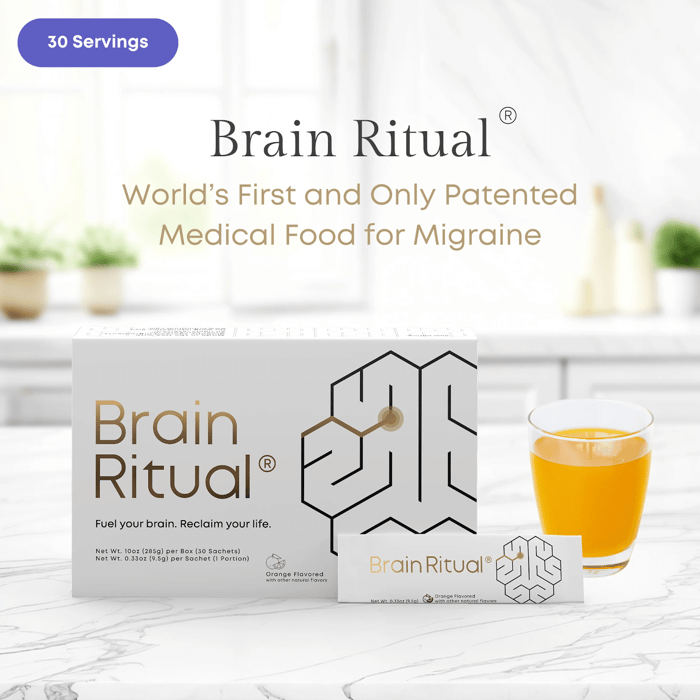
For women navigating both birth control and migraine, here's why this approach deserves attention:
Aspect | How It Works | Practical Application |
Addressing the "Double Hit" Effect | Brain Ritual provides alternative fuel (ketone bodies/BHB) when hormonal fluctuations deplete brain energy, helping stabilize metabolism during vulnerable periods | Track migraine patterns in relation to your contraceptive cycle to identify when you need to be most diligent with your Brain Ritual regimen |
Compatibility | Contains no hormones and works through different mechanisms than contraceptives, making it suitable alongside progestin-only or non-hormonal methods | Can be used daily without interfering with your chosen birth control method |
Transitional Support | Supports a strong brain energy baseline, which can help to cope better with birth control method changes (potential migraine triggers) | Consider using consistently when switching contraceptive methods to build resilience against transition-related triggers |
Complementary Mechanisms | While birth control addresses hormonal aspects of migraine, Brain Ritual targets suboptimal metabolism | Discuss with healthcare providers how to coordinate timing of both approaches for maximum benefit |
The most successful approach combines appropriate birth control with complementary strategies like Brain Ritual to address different aspects of migraine physiology.
Consider discussing with your healthcare provider how to integrate:
Your selected migraine-friendly birth control method
Medical food supplementation targeted at brain metabolism
Rescue medications if needed
By thoughtfully combining these approaches, you're not just avoiding pregnancy, you're creating a comprehensive strategy to lower both the frequency and severity of migraine attacks while maintaining reproductive autonomy.
Remember that the right approach is highly individual. What works perfectly for someone else might not be ideal for you.
The goal is finding a personalized approach that lets you manage both your reproductive health and neurological wellbeing effectively.
Frequently Asked Questions
Now that we've explored birth control options for migraine sufferers, let's address some common questions
Can switching to a low-dose estrogen pill minimize migraine attacks?
Many women with migraine without aura wonder if lower concentrations of estrogen might help their condition.
Some contraceptive formulations with lower doses of estrogen may indeed be better tolerated than high-dose pills for those experiencing migraine without aura.
The theory is that smaller fluctuations in hormone levels might trigger fewer headaches.
However, this approach is only suitable for women without migraine aura and with no additional risk factors for cardiovascular diseases or venous thrombosis.
If you have a history of migraine with aura, even low-dose combined hormonal contraceptives still carry an increased risk for stroke and are not recommended.
Always discuss the frequency of headaches in relation to your menstrual period with your healthcare provider to determine if a lower estrogen formulation might be appropriate for your condition.
How does the drop in estrogen levels during my cycle affect migraine patterns?
The relationship between female hormones and migraine attacks is well-established.
Many women experience what's called "menstrual migraine" due to estrogen withdrawal that occurs just before their period begins. This drop in estrogen levels serves as a powerful trigger for those susceptible to hormone-related headaches.
Combination birth control pills, the transdermal patch, and vaginal rings all create artificial cycles that include an estrogen withdrawal phase during the hormone-free interval.
For some women, this drop in estrogen levels during the placebo week can actually worsen migraine patterns.
Extended or continuous use of hormonal birth control pills (skipping the placebo week) might help minimize these estrogen-withdrawal headaches by eliminating the drops in estrogen levels that trigger attacks.
This approach can be particularly helpful for women whose migraine diary reveals a clear pattern of headaches during hormone fluctuations.
Is progesterone-only pill (mini-pill) safer than combination birth control pills if I have a history of migraine with aura?
Yes, the progesterone-only pill (also called the mini-pill) is considered significantly safer than combination birth control pills for women with a history of migraine with aura.
Unlike combination pills, the mini-pill contains no estrogen, which is the hormone associated with increased risk for stroke and blood clots in migraine with aura patients.
The mini-pill works primarily by thickening cervical mucus and thinning the uterine lining, providing good protection against unintended pregnancy without elevated estrogen levels.
While it requires more consistent timing than combination pills (it must be taken within the same 3-hour window daily), this type of birth control offers a safer alternative for migraine sufferers with aura.
However, even the mini pill still raises oxidative stress and might increase migraine threshold and risk over longer periods of time.
Can an intrauterine device (IUD) affect the frequency of migraine attacks?
The impact of an intrauterine device (IUD) on migraine frequency depends on the type you choose.
The copper IUD contains no hormones whatsoever and therefore doesn't directly influence migraine patterns through hormonal mechanisms.
This makes it an excellent option for avoiding unintended pregnancy in women with any type of migraine, including those with aura who need to avoid estrogen completely.
Hormonal IUDs (containing only progesterone) primarily work locally within the uterus, releasing much lower amounts of hormone into the bloodstream compared to other forms of hormonal contraception.
However, some women still experience changes in headache patterns as this still impacts endogenous hormone production, so it can carry risk as well.
Is it safe to use hormonal birth control for migraine during perimenopause?
Using hormonal birth control during perimenopause requires careful consideration for migraine sufferers.
Perimenopause often brings wildly fluctuating hormone levels that can increase migraine frequency, and many women consider hormonal therapy to stabilize these fluctuations.
However, the combination of age (typically over 35), migraine history, and estrogen-containing contraceptives significantly increases the risk for cardiovascular complications, including deep vein thrombosis and stroke.
For perimenopausal women with migraine with aura, estrogen-containing methods are generally contraindicated regardless of potential benefits for symptom control.
Progesterone-only contraceptives or non-hormonal options like the copper intrauterine device remain safer choices for avoiding pregnancy during this transition.
Some physicians may consider carefully monitored, very low-dose bioidentical hormone replacement therapy specifically designed for perimenopausal symptom management (different from contraceptive formulations) is much better
Conclusion
If you experience migraine with aura, progestin-only methods and non-hormonal options like the copper IUD offer safe alternatives to estrogen-containing contraceptives that increase stroke risk.
For those with migraine without aura, more options exist, including carefully selected low-dose combined hormonal methods.
However, all hormonal contraceptives increase oxidative stress and thereby may negatively impact migraine risk and threshold in the long-run, so risks and benefits should be carefully evaluated when choosing hormonal contraception in migraine.
The ideal approach is highly individualized, what works perfectly for someone else may not be right for you.
Working closely with healthcare providers who understand both reproductive health and migraine management is essential.
By tracking your symptoms, being transparent about your migraine history, and considering complementary approaches like medical foods, you can find a contraceptive approach that protects both your reproductive autonomy and neurological wellbeing.
Remember that finding the right method may take time and patience, but safe options exist for every migraine sufferer, regardless of your specific headache pattern or risk factors.




